What to do with an Achilles Tendon Injury?
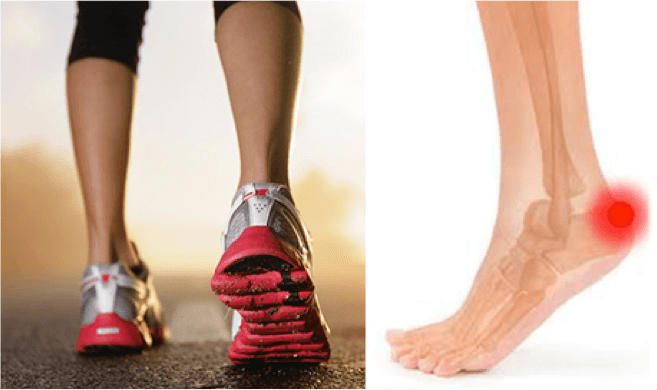
Achilles tendinopathy – the curse of the ageing athlete?
By Peter Georgilopoulos APA Sports Physiotherapist
A recurrent problem facing many elite and recreational runners is Achilles pain and stiffness.
Previously, this has been described as ‘Achilles tendonitis’ which refers to inflammation, micro-tearing and scarring of the Achilles tendon. Improved investigative procedures however have shown that the causes of pain may not be limited to the Achilles tendon alone but may extend to surrounding structures as well. The wider spectrum of damaged structures is therefore better describes as ‘Achilles tendinopathy’.
The condition is also characterised by morning stiffness or stiffness following prolonged immobility and eased by gentle movement which is often associated with ‘cracking’ or ‘grinding’ of the tendon. The lack of movement overnight allows inflammatory fluid to surround the tendon and its sheath causing an audible or palpable grinding sound on activity.
Frequently, symptoms may be linked to increased mileage and rest is often sufficient to alleviate pain. In other cases however, minor pain can progress to severe dysfunction resulting in an inability to continue training.
Recurrent Achilles inflammation can lead to excessive scarring and consequent tendon thickening. As the tendon is reliant on surrounding fluid for nutrition and sustenance, a thickened tendon can lead to atrophy of its core and can significantly increase the risk of sustaining an acute full thickness rupture if placed under sudden stress.
Ultimately, irrespective of the specific site or extent of pathology, there are two treatment considerations that need addressing;
- Reduction of inflammation and promotion of cellular repair.
- Evaluation and correction of the underlying biomechanical causes that have enabled excessive loading and breakdown to occur.
Although Achilles tendinopathy commonly affects senior athletes, it is simplistic to believe that the onset is somehow the result of ageing tendon structures alone. Age does not explain why symptoms may present intermittently and disappear for lengthy periods or why it may appear on one limb but not the other.
What causes Achilles tendinopathy?
The simple answer is – excessive loading over prolonged periods will result in micro-tears, inflammation and pain. The vital question should be – “what causes excessive loading in the first place?” The most common causes are:
- A sudden increase in exercise intensity, frequency, type or duration.
- Tight calves – a lack of flexibility in the calf complex leads to excessive tensile force through the tendon leading to microscopic tears.
- Asymmetrical loading of the tendon as a result of flat feet. Angulation of the Achilles tendon due to flat feet means that the inner half of the tendon receives far greater load because it is “stretched” over a greater distance than the outer aspect of the tendon.
- Inappropriate or unsupportive footwear.
- Running on hard surfaces.
- Growth spurts leading to limb length discrepancy (relevant to juvenile athletes only).
- Knock kneed deformity which forces the feet into a flat footed posture altering the distribution of load bearing capacity throughout the Achilles tendon.
- Bow legged deformity creates excessive flat footed posture which allows maximal sole contact of the foot with the ground.
Management of Achilles tendinopathy
The primary objective should be obtaining an accurate diagnosis and causative factor(s) by a qualified professional. Depending on the identified causative factors, management may include:
- Restoration of flexibility of the calf and/or hamstrings. Exercises may include straight leg raises, calf stretches and ankle lunges. Aim to achieve symmetry of the affected and non affected limbs.
- Biomechanical correction may be achieved through changing to more supportive running shoes, orthotic devices, heel lifts or running gait analysis.
- Symptomatic relief can be achieved through rest from provocative exercise, ice after activity, non steroidal anti-inflammatory medication and manual and electrotherapy modalities.
- Eccentric exercise (use arms to lift body to a toe point position then slowly return to neutral using full body weight).
- Cortisone or PRP (plasma enriched protein) injections might be recommended by your physician. Benefits and possible complications need to be discussed prior to selecting these options.
Achilles tendinopathy need not be the curse of ageing athletes – maintaining good flexibility, wearing supportive footwear and moderating exercise intensity with sufficient rest between sessions should enable symptom free activity throughout your athletic career and beyond.